Seventh grade is when I officially grew up.
On a weekday afternoon after school had gotten out, my nurse directed me into a random room and told me to have a seat while she went over my medical history. I looked at my mom who was sitting in the seat right next to the nurse’s computer to get the nod off that I was giving the nurse all the correct answers to her questions I had memorized just from going to the doctor’s so much. After the nurse left, my mom and I waited patiently. It was a typical day for me. Going to the doctor’s after school or even sometimes during school. I expected the same response from my doctor to be that they did not know what was wrong with me and that they could refer me to someone who did. I had lost track of how many referrals I had been through.
My doctor came in and went over my symptoms and the pain I was experiencing in my lower abdomen. He was kind and funny, but he laid it on me thick when he was the first person to tell me it would be extremely difficult and painful for me to have kids. I just stared back at him blankly and nodded. I felt gutted but I swallowed the lump in my throat and refused to let one tear hit my cheek.
I had officially grown up.
I went home, headed to my bedroom and closed the door. I looked around my room and felt like I no longer belonged. I was no longer the awkward tween girl that still played with her American girl dolls and had her purple canopy over her bed, I was the young woman who was told her dreams of being a mother someday felt too hard and painful to achieve.
As I grew up, my condition only got worse. Like many women have experienced, I was not taken seriously. I was told that my extreme pain and heavy bleeding were symptoms of my period. After years of feeling the same, I knew that my pain was not just because of my period. Nothing had changed no matter how many methods of medication I tried.
My sophomore year of college was just like seventh grade, a time of change. I felt sluggish and weak, going through work and school like a zombie. My hair got thin and brittle, my eyes carried bags under them and my skin was paler than usual. I found myself isolating from my loved ones because I refused to let those around me be affected by the pain I was enduring. I put on a front that I was strong and that I could handle it when I was dying inside.
After a lot of trial and error, I eventually found a doctor that saw right through me. She saw how badly I was struggling and how much I was keeping inside. She didn’t downplay it or normalize it. She saw me.
Now here I am after ten years with a name to my diagnosis.
My endometriosis scars on my stomach. Photo credit to Claire Plath.
My endometriosis scars on my stomach. Photo credit to Claire Plath.
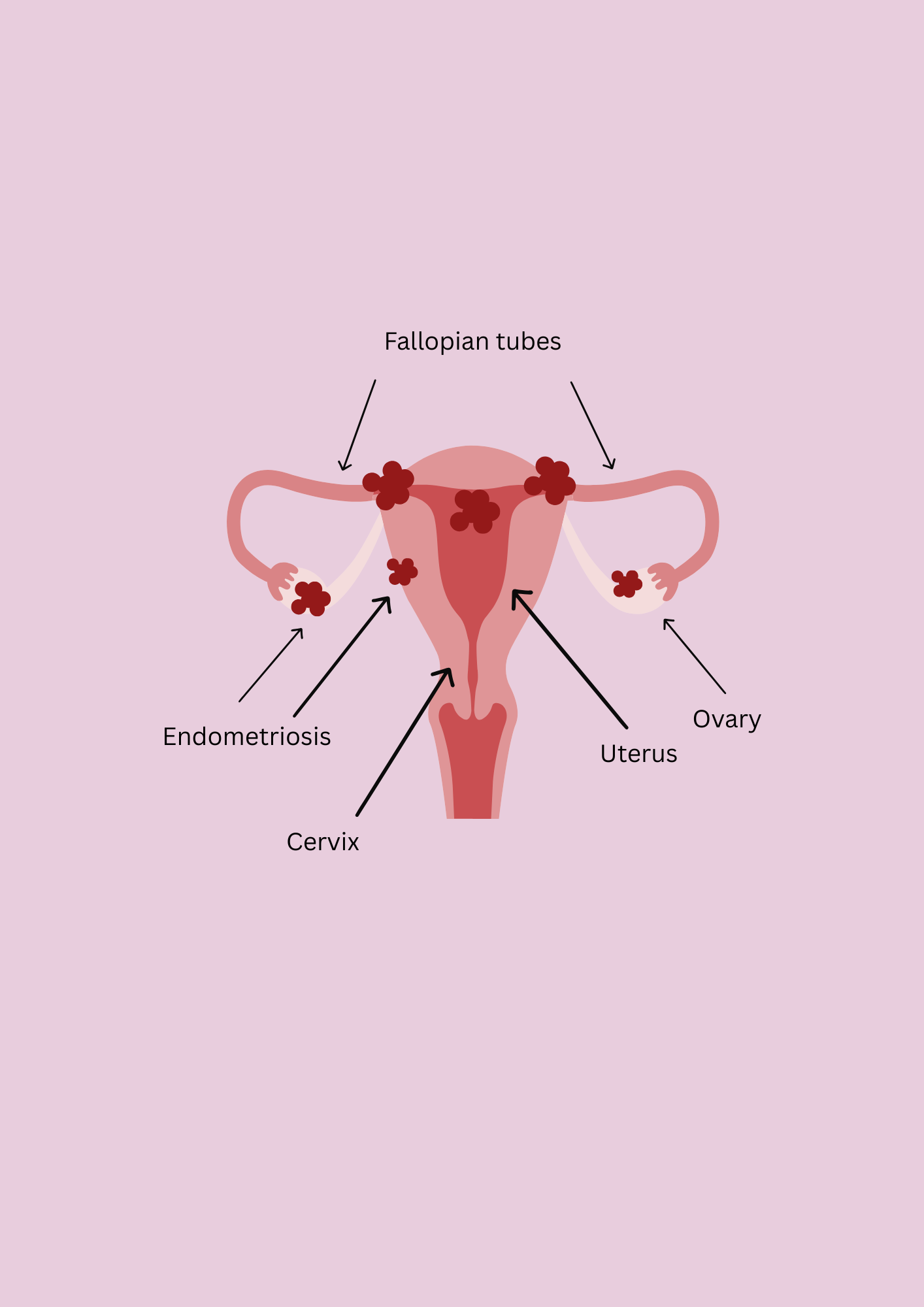
Endometriosis - what is it?
Endometriosis is a disease in which tissue similar to the lining of the uterus, grows outside of it in places that it does not belong. It can grow in the ovaries, in your back, bladder, rectum, on the bowels and can even spread to other destinations of the body, creating lesions. The tissue is hormonally responsive as estrogen will stimulate that lesion to grow.
It is a misplaced, inflammatory tissue that causes severe pain, heavy periods, infertility and more agonizing symptoms.
Doctors classify endometriosis based on stages 1 through 4. The stages are based on where the endometriosis tissue has spread to in the body and how excessive that spread is.
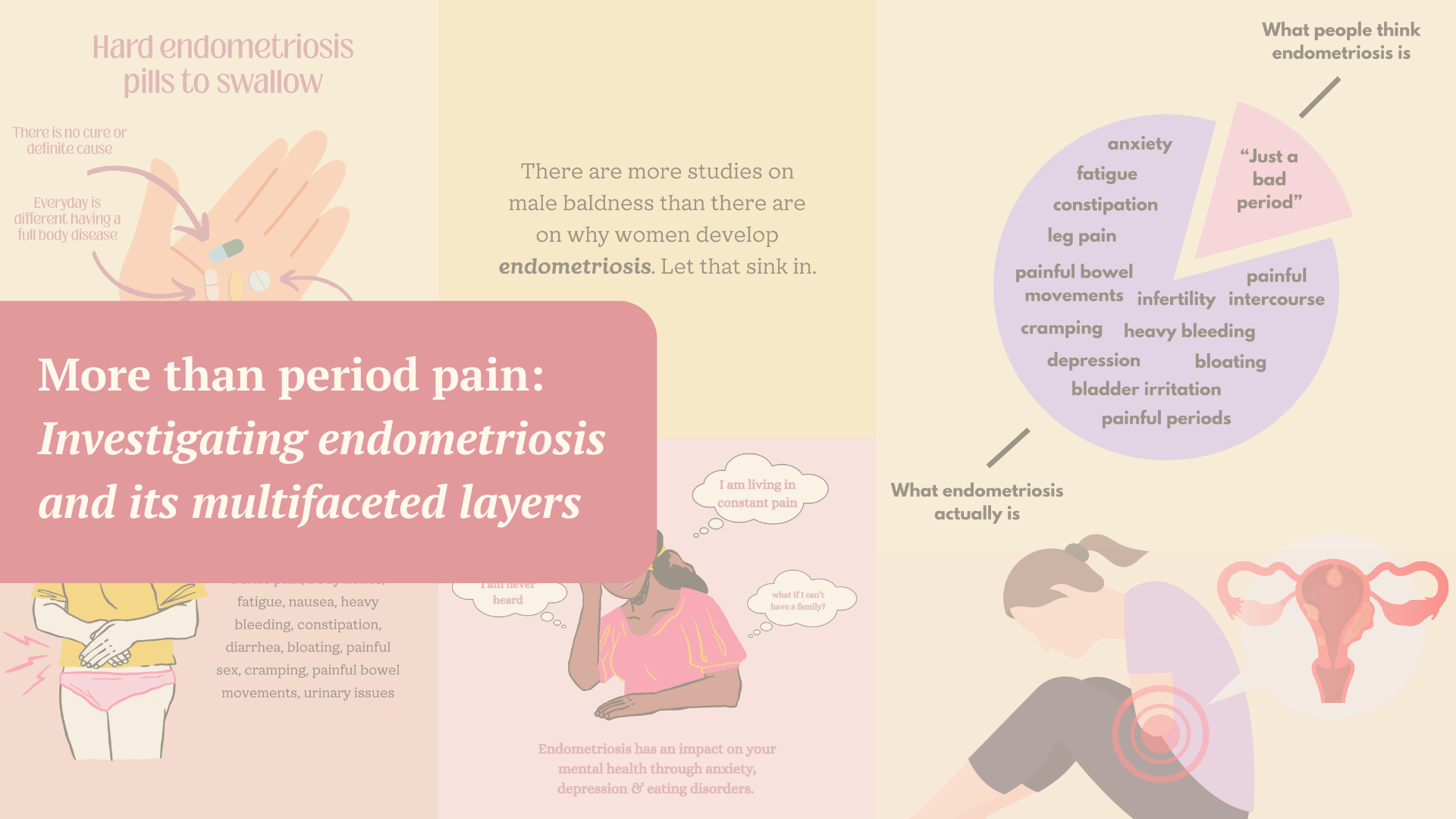
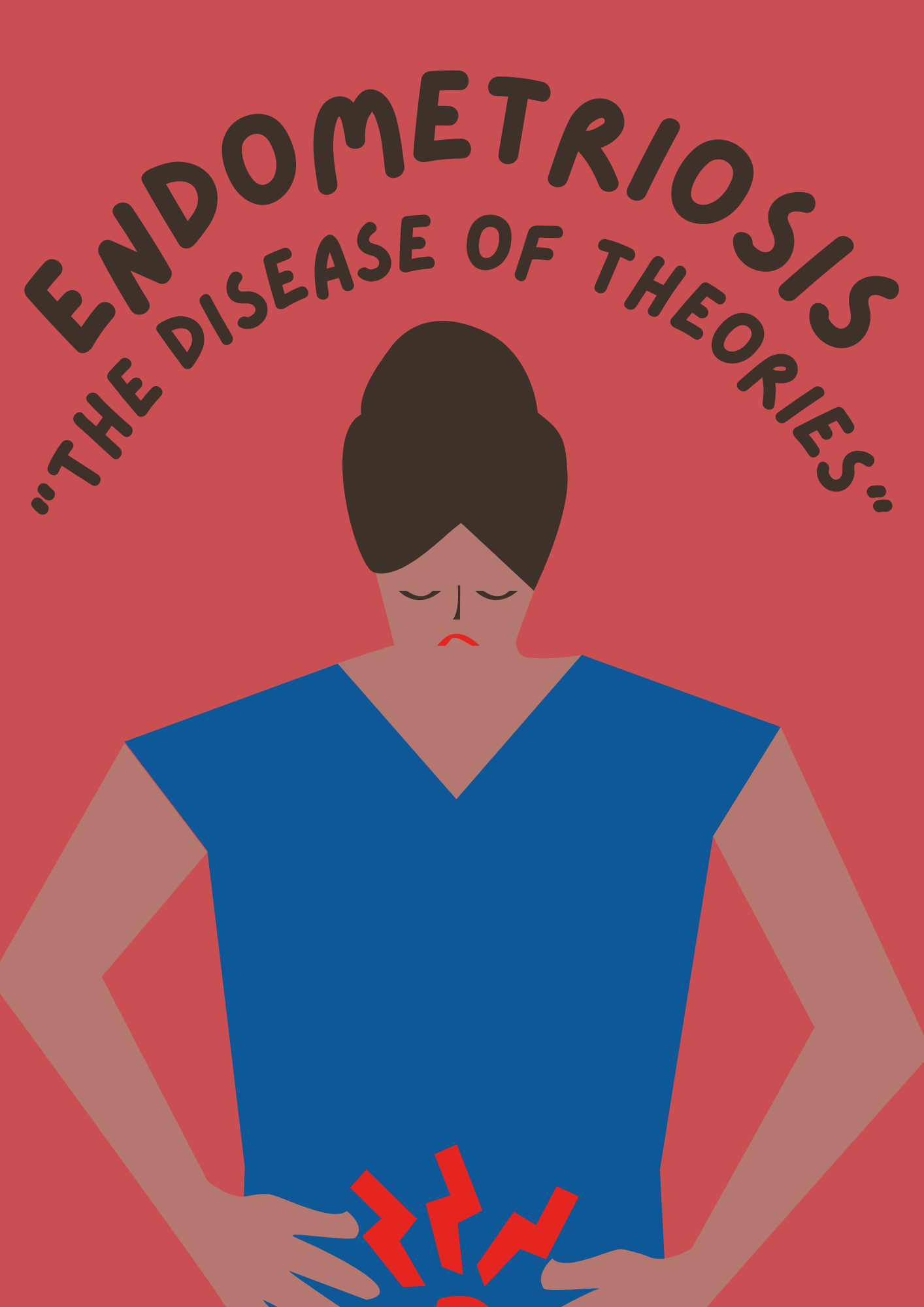
Endometriosis affects roughly 10% of reproductive age women globally.
Even though a woman can have stage 1 endometriosis, it does not mean that their symptoms are not as severe. Someone with stage 1 can have worse symptoms than someone with stage 4 endometriosis.
10% of women of reproductive age (15-49 years old) have endometriosis, but the age that a woman can develop endometriosis varies. This adds up to roughly 190 million women worldwide.
The cause of endometriosis is unknown, there is no way to prevent it and there is no cure.
Physical symptoms of endometriosis include:
Pain, pain, pain.
Infographic made by Claire Plath.
Infographic made by Claire Plath.
Where does it come from?
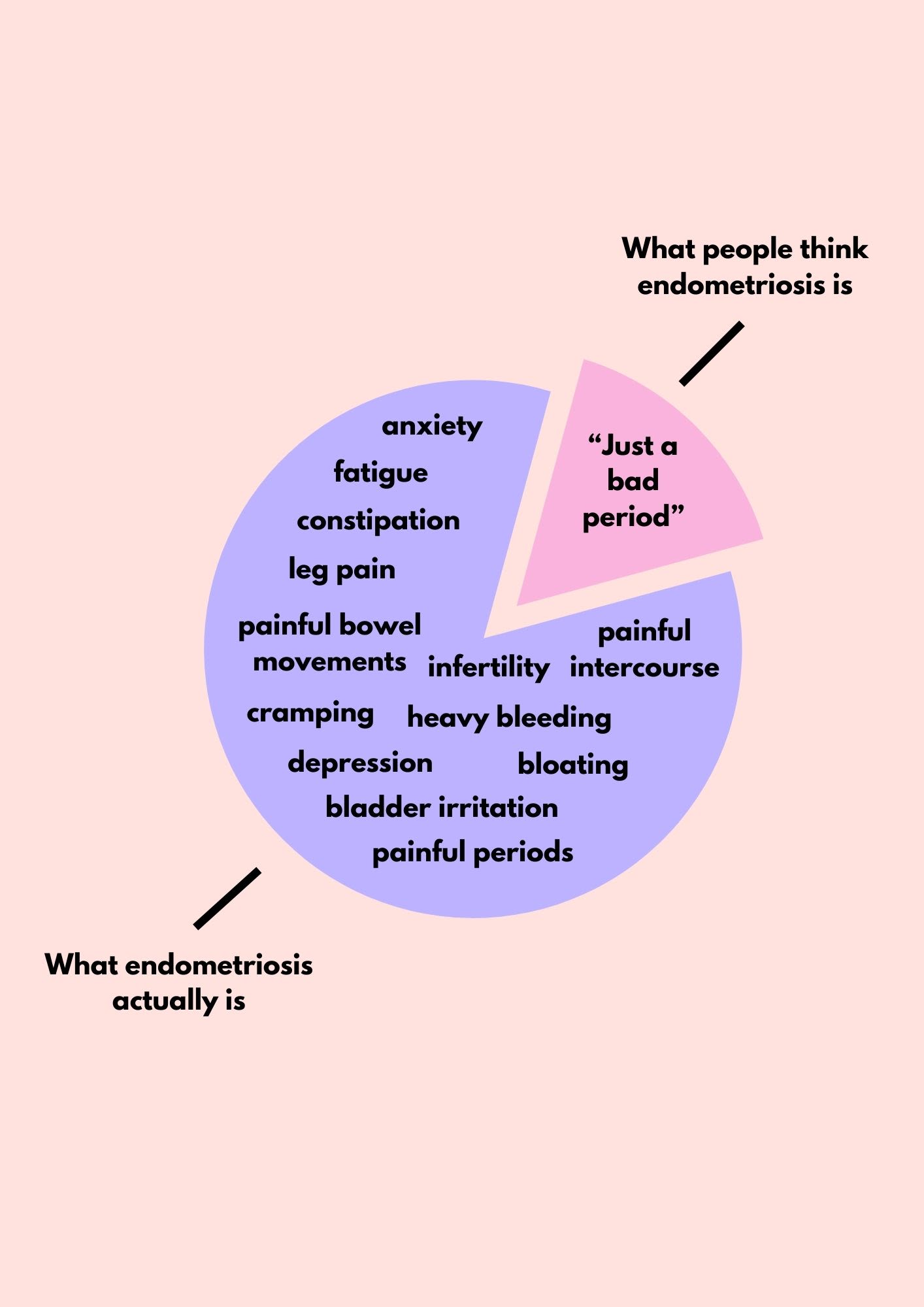
The truth is, no one knows for certain where endometriosis comes from. Endometriosis is often referred to as “the disease of theories.” There are theories about where it is derived from, but nothing is confirmed.
A few of these theories include:
Retrograde menstruation: During a period, instead of all of the menstrual blood coming out from the cervix to the vagina, it is spilling out the fallopian tubes into the abdomen leading to the implantation of endometrial cells.
The embryological theory: through development of the embryo into a fetus, the tissue that is meant to live in the uterus is getting lost and developing into different areas of the body. There have been endometriosis lesions found in unusual places outside of the uterus like the spine or around the heart as to why this is a suspected theory.
Spread through the lymphatic system: This theory suggests that endometrial cells are traveled and spread through the lymph nodes all around the body, but this case is typically unusual.
There is also the question if endometriosis is affected by an environmental impact. However, it is unknown and uncertain if there will ever be an answer of where endometriosis comes from.
Dr. Holly Kawano is a board certified OB/GYN at St. Luke’s Hospital located in Boise, Idaho.
Dr. Kawano graduated from medical school at the University of Washington and went on to complete her residency training in Rochester, New York. She landed her first job at St. Luke’s and has now been there for over 12 years.
When Dr. Kawano was doing her residency back in 2012, she said endometriosis was misunderstood and under-appreciated. She went to a residency that had a great pelvic pain program who recognized the importance of it, but it was still under-managed.
Since then, Dr. Kawano has a lot experience with patients who have been diagnosed with reproductive health issues, including endometriosis. She still acknowledges how complex of a disease endometriosis is today.
“Endometriosis is a really difficult diagnosis and what is so difficult about it is how unrecognized it is. It is something a lot of women suffer from and don’t even realize they are suffering from it,” said Dr. Kawano.
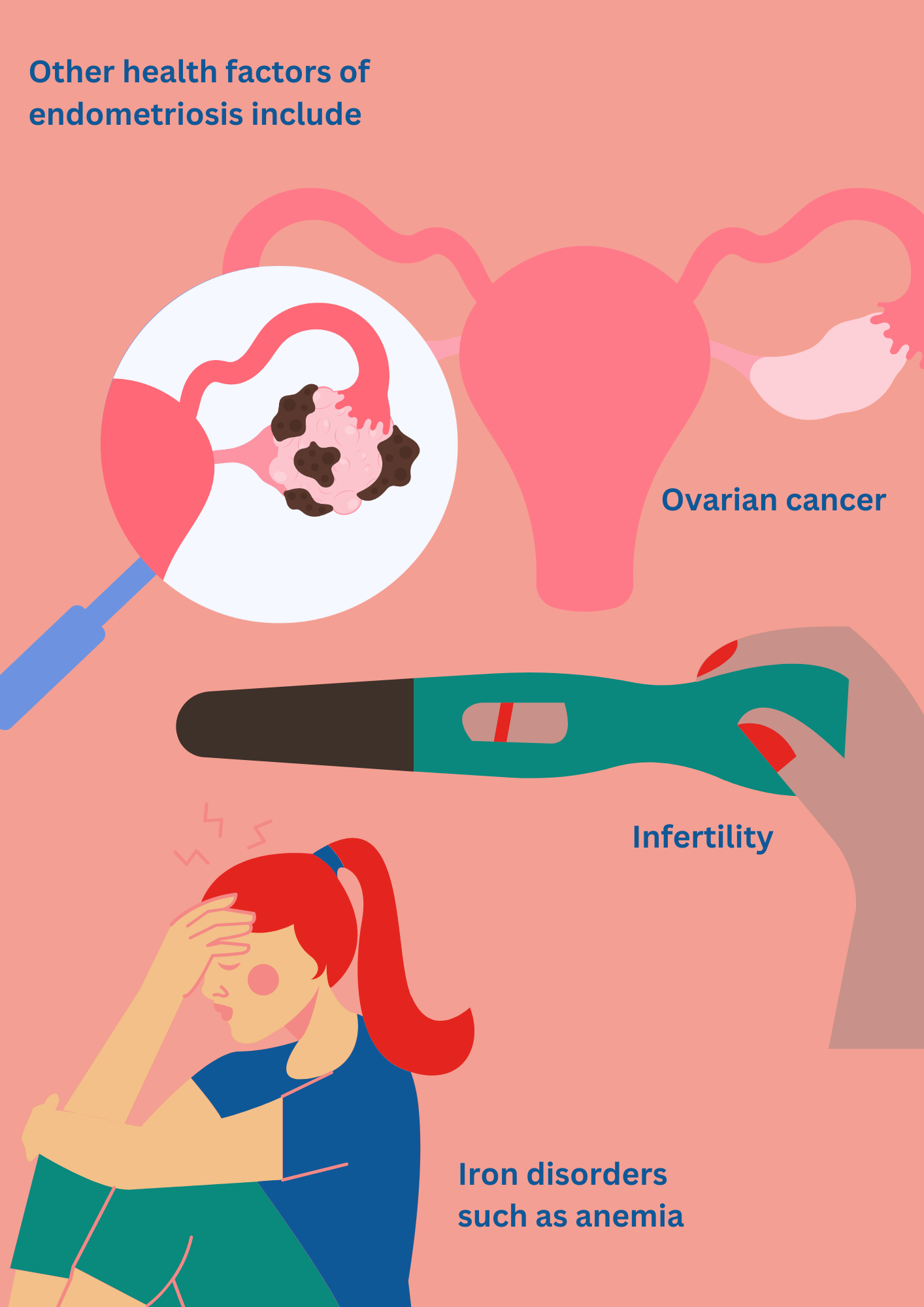
Other health factors
Ovarian cancer
Women with endometriosis are suspected to be linked to other health and risk factors, a common one in particular being ovarian cancer.
The National Library of Medicine conducted a study in 2024 that shows how endometriosis raises the risk of ovarian cancer. Researchers in Utah looked at 79,000 women with endometriosis, comparing them to women without it. They narrowed their research down based on the stages of endometriosis. Their findings concluded that women with endometriosis are more likely to develop ovarian cancer type I. Type I ovarian cancer is when slow growing tumors arise from benign lesions like borderline tumors or endometriosis.
Women with deep infiltrating endometriosis had the highest risk for developing type I ovarian cancer, with a probability of 19 times higher.
This research shows that the different stages of endometriosis significantly increase the risk of type I ovarian cancer.
"Endometriosis is a really difficult diagnosis and what is so difficult about it is how unrecognized it is. It is something a lot of women suffer from and don’t even realize they are suffering from it."
Iron disorders
Endometriosis is associated with other health risks such as iron disorders.
Women with endometriosis often experience heavy or irregular periods, leading to significant blood loss. The excessive loss of blood can result in iron deficiency and anemia.
Iron is extremely important for the body because it plays a crucial role in the production of red blood cells which carry oxygen throughout the body. Low iron levels have similar symptoms to endometriosis when it comes to feeling fatigue, having low energy and a poor appetite.
Endometriosis can cause chronic inflammation and heavy menstrual bleeding which can result in iron deficiencies with the body’s inability to absorb iron properly. Another study from the National Library of Medicine confirms that iron loss during heavy menstrual bleeding is one of the most common reasons for iron deficiency in women.
Infertility
Endometriosis is also a common cause of infertility. Endometriosis causes inflammation, scarring and distortions in the pelvic area from its lesions. It can interfere with a woman’s fallopian tubes and ovaries when it implants on them, making it much more difficult for a woman to get pregnant.
It is also more difficult for people with endometriosis to get pregnant. The online article “Endometriosis and its Impact on Fertility” from the Massachusetts General Hospital in 2023 details how endometriosis impacts a woman’s fertility.
The article says, “Endometriosis has also been shown to alter the immune system, change the hormonal environment around the eggs, inhibit implantation of an embryo and alter the quality of the eggs.”
Photo graphic made by Claire Plath.
Photo graphic made by Claire Plath.
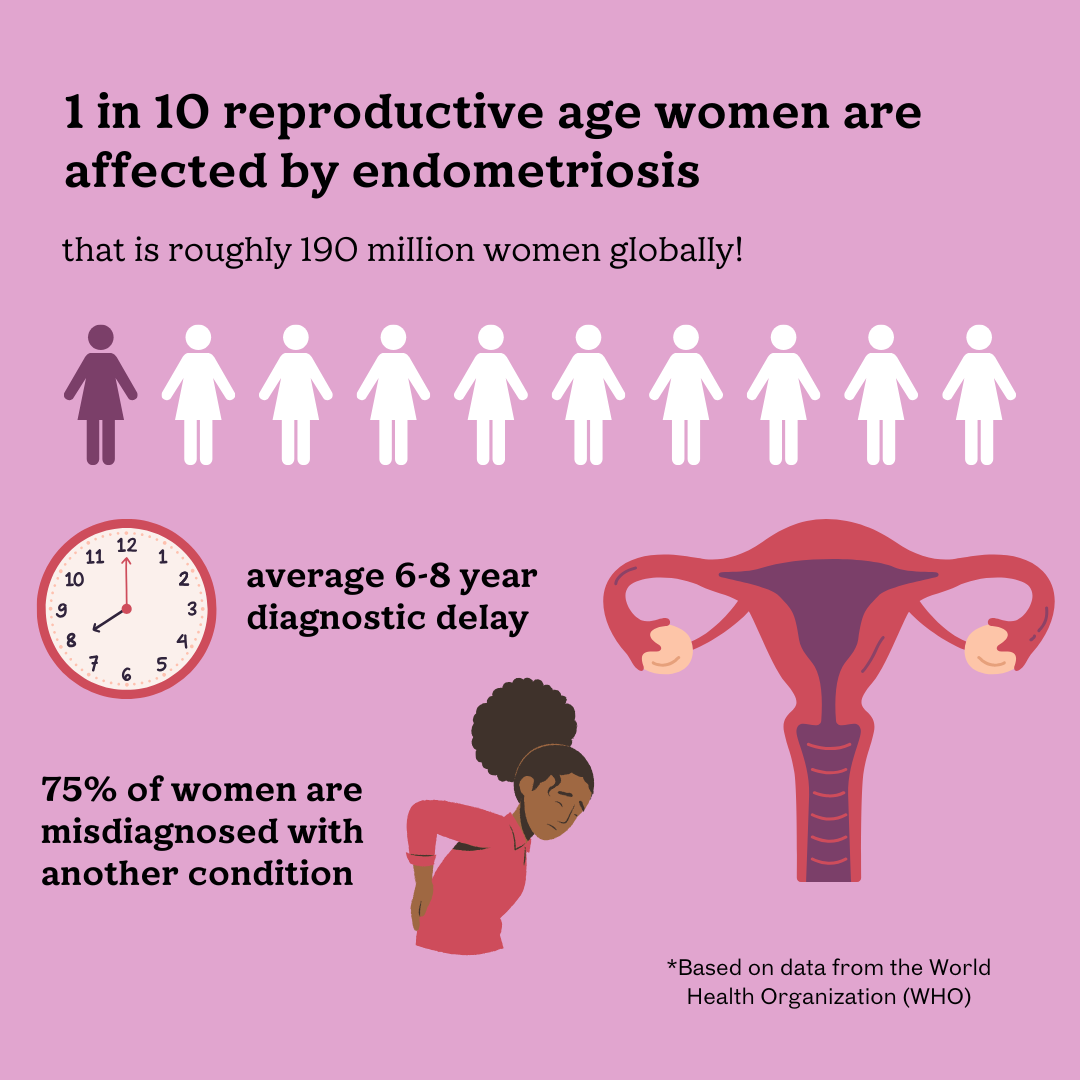
Endometriosis symptoms graphic, made by Claire Plath.
Endometriosis symptoms graphic, made by Claire Plath.
"The disease of theories" graphic made by Claire Plath.
"The disease of theories" graphic made by Claire Plath.
Diagram showing endometriosis growth, made by Claire Plath.
Diagram showing endometriosis growth, made by Claire Plath.
Other health factors of endometriosis graphic made by Claire Plath.
Other health factors of endometriosis graphic made by Claire Plath.
Rachel Ratelle
Rachel Ratelle, a 23-year-old University of California San Diego alumna, was recently with endometriosis after eight long years of trying to figure out what the cause of her pain was. She is the founder of "Rays Your Vibe," an organization that is all about endometriosis awareness and creating community for women who have endometriosis.
1869 portrait of "Witch Hill." Photo courtesy of Wikimedia Commons.
1869 portrait of "Witch Hill." Photo courtesy of Wikimedia Commons.
"Examination of a witch" portrait from 1853. Photo courtesy of Wikimedia Commons.
"Examination of a witch" portrait from 1853. Photo courtesy of Wikimedia Commons.
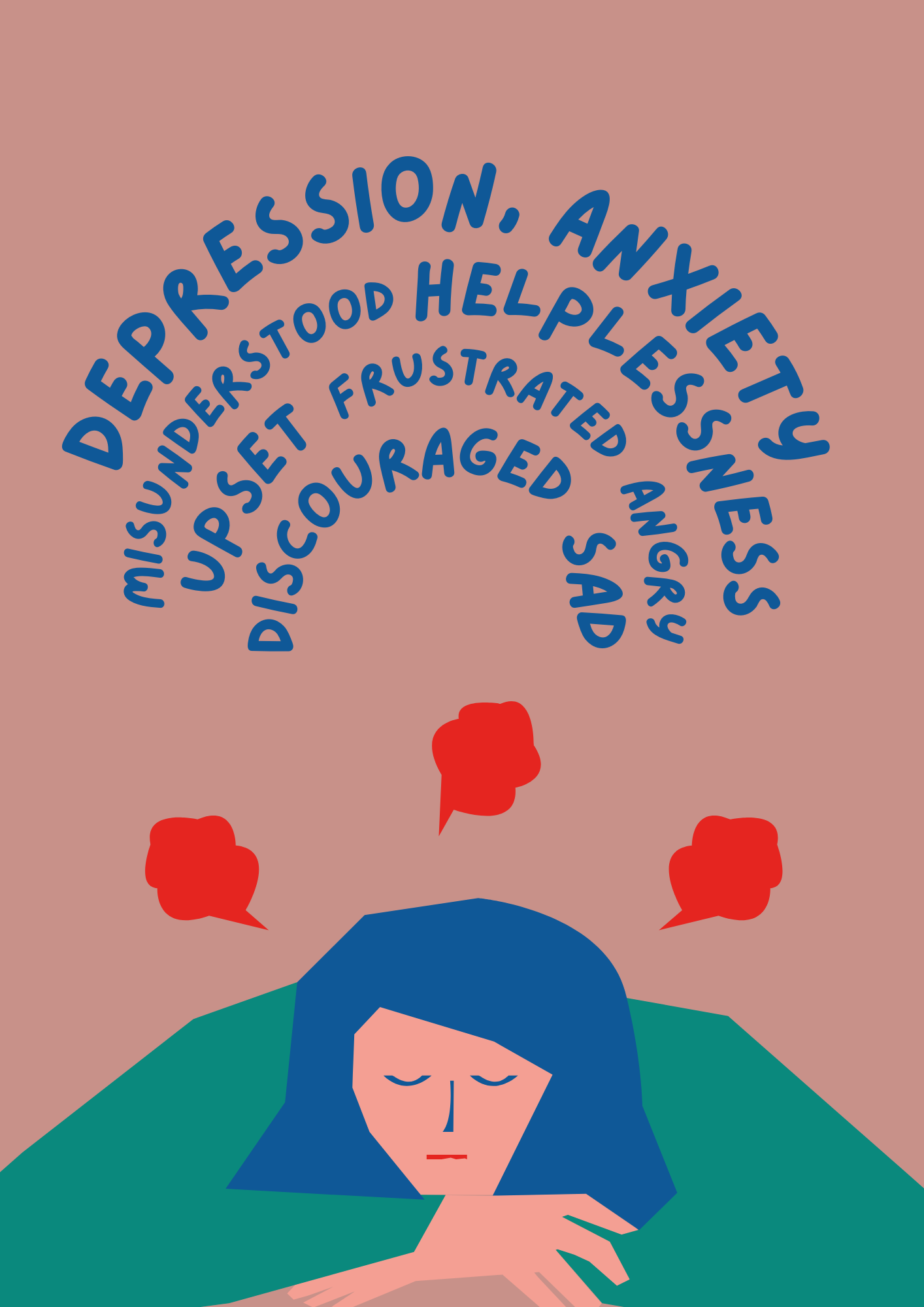
Endometriosis mental health impact graphic made by Claire Plath.
Endometriosis mental health impact graphic made by Claire Plath.
Dyspaurenia graphic made by Claire Plath.
Dyspaurenia graphic made by Claire Plath.
Mental health impact & history of women’s “hysteria”
The debilitating physical pain that comes with endometriosis bleeds into the mental and emotional well being of a woman with the disease, which has been an ongoing issue throughout history.
For centuries, women were misdiagnosed and mistreated for their reproductive health problems. In ancient Greece, doctors practicing in the Hippocratic tradition blamed women’s health problems (infertility, pain, depression, anxiety) on “hysteria,” where they were under the pretense that the uterus was wandering around the body.
Treatments for a woman’s hysteria were harmful and even included hanging women upside down while shaking them to “put the uterus back in place.”
The common theme of hysteria for women has continued throughout time, and women were harshly punished for it. The Yale School of Medicine article “From hysteria to empowerment” states: “Women were accused of madness, witchcraft, or demonic possession, and forced to undergo exorcisms, burned as witches, or confined in mental institutions.”
During the Victorian era, more disturbing treatments were being conducted where doctors during this time, stimulated their female patients through “pelvic massages” until they reached orgasm, as a cure for their “hysteria” and the reproductive health problems they were facing.
It was not until the mid 19th and 20th centuries, with the emergence of the first wave of feminism, that women began to consistently advocate for themselves and put an end to the hysteria myths.
There have been significant improvements in advocacy for women’s reproductive health and rights, but there are still challenges women face.
“Historically, when women had trouble with menstrual cycles or pain, or whatever it was, they were considered hysterical."
Chronic pelvic pain is linked to depression and anxiety. Women with endometriosis are twice as likely to suffer from a mental health condition. It can decrease the quality of life for a woman due to the major symptoms of pain, anxiety, depression, fatigue and more that come from it.
One example is the endometriosis symptom of painful intercourse (also known as dyspareunia) which affects a person’s mental and emotional health. A study was conducted where 2,060 women diagnosed with endometriosis, average age of 30, filled out a questionnaire assessing sexual pain and distress due to the disease. Approximately 80% reported that endometriosis negatively impacted their sex lives with 68% experiencing severe sexual distress because of it.
Dyspareunia negatively affects a woman’s quality of life as another common symptom women with endometriosis endure.
Women often have to wait an average of 6-10 years for a diagnosis of endometriosis. It is a common pattern for women to be dismissed by their doctors and for their symptoms to be undermined. Endometriosis itself is extremely painful and consuming, causing a woman’s mental and emotional health to worsen.
“It leads to a trickle down effect on how it impacts a woman’s mental health, where I tell people all the time, just the validation of their symptoms is huge. Like the weight you can just watch, lift off of their shoulders when you tell them you believe them and that you can do something to help them,” said Dr. Kawano. “This has become one of the greatest joys of what I do. Just watching people finally feel validated in their symptoms.”
Women need to be heard, understood and validated for their struggles.
How endometriosis is prevalent in families

Genetic Factors
There is a trend with endometriosis running in families and it has been suspected that it may be hereditary. Yet there has not been one specific gene that connects to endometriosis, leaving it unknown if it actually is.
“One thing I noticed in my patient population is family history. I think there is a link in family history, I think if you have a mom, a sister, an aunt and a cousin who all had endometriosis and you're experiencing pelvic pain, it's pretty likely that endometriosis is high on that differential,” said Dr. Kawano.
Scientists from the University of Oxford in 2023 along with 25 other researchers from around the world, conducted one of the largest studies on the genetics of endometriosis to see if there may be a link. They looked at the DNA of over 60,000 women with endometriosis and 700,000 without it. They discovered that endometriosis as well as other kinds of pain such as migraines, may share some of the same genes.
The study confirmed the theory that certain genetic differences called variants can make someone more likely to develop the disease. By comparing the DNA of women with and without endometriosis, the researchers found 42 spots in the genome that are linked to a higher probability of getting it.
In simpler terms, if your mom, sister or close relative has endometriosis, you are more likely to get it too. This specific study is a huge step in discovering if there are biological causes to endometriosis. More research needs to be conducted in order to validate these studies and theories.
This is relevant in my own family. My grandmother and my mother both had endometriosis, and now it is passed down to me. Their stories of endometriosis have shaped them into the strong, persevering women they are.
Listen below to hear both my grammy's journey and my mother's journey with endometriosis through the decades.
Photo collage of Shirley Hackett (my grammy) and Cammie Plath (my mom) through the years. Photo courtesy of Hackett and Plath.
Photo collage of Shirley Hackett (my grammy) and Cammie Plath (my mom) through the years. Photo courtesy of Hackett and Plath.
"You just had to learn to live with endometriosis."
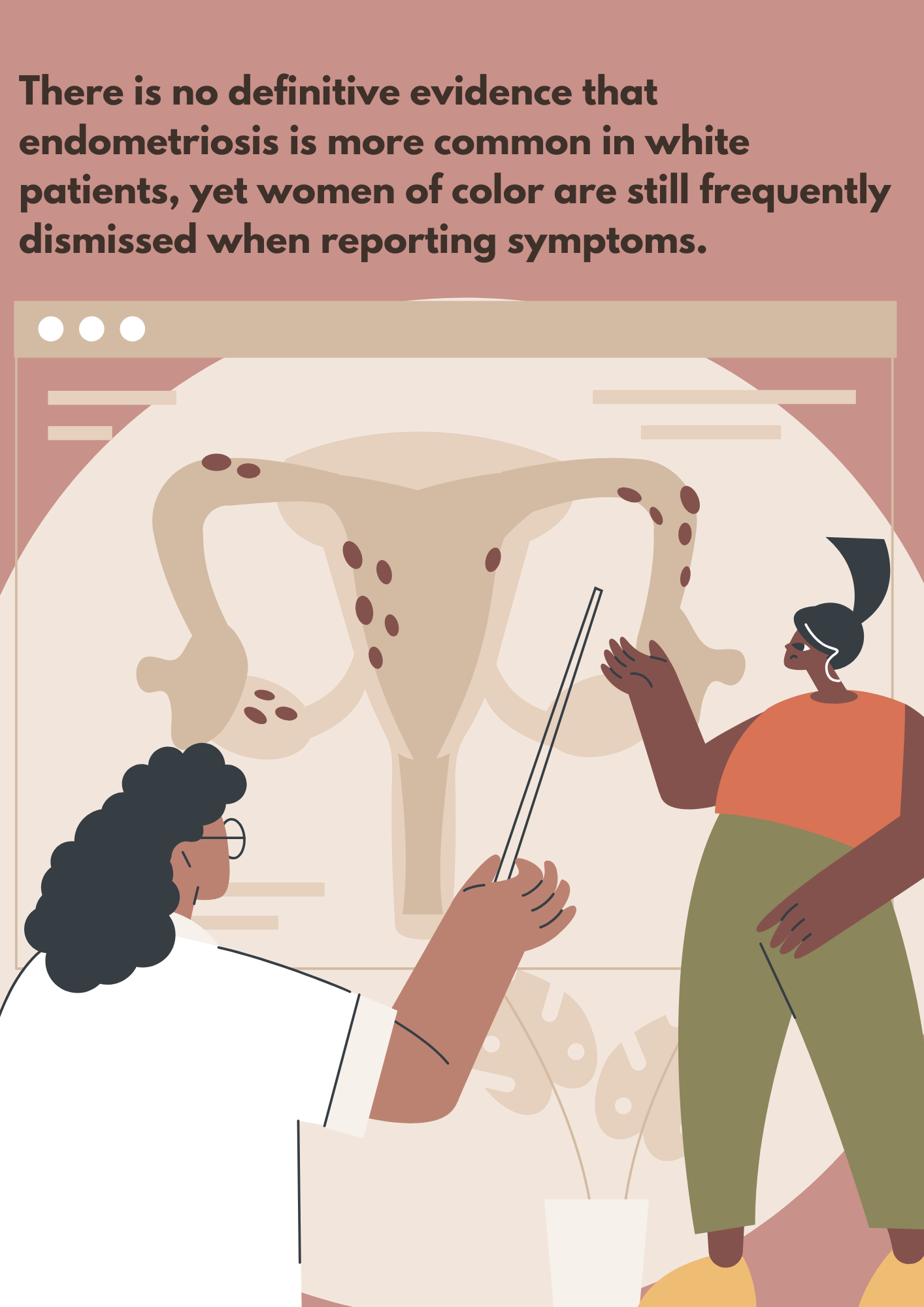
Racial disparities graphic made by Claire Plath.
Racial disparities graphic made by Claire Plath.
J. Marion Sims the "father of gynecology." Photo courtesy of New York Public Library's public domain archive.
J. Marion Sims the "father of gynecology." Photo courtesy of New York Public Library's public domain archive.
Racial disparities
Racial disparities exist and are prevalent in the diagnosis and treatment of endometriosis. Black women continue to receive poorer care for endometriosis and are often misdiagnosed.
Racial prejudices go back to the history of gynecology, with “the father of gynecology” Marion J. Sims, who experimented on enslaved Black women, exploiting their bodies for gynecology purposes during the 19th century.
The experiments and surgeries were performed without anesthesia or medical pain reducers, due to the fact that Sims cared more about the experiments he was conducting rather than the treatment of Black women. He performed his experiments under the belief that Black people felt no pain.
Sims invented the vaginal speculum, a tool used for dilation and other surgical techniques to help treat complications during childbirth. Yet there is no evidence that the Black women he performed these examinations on, gave consent.
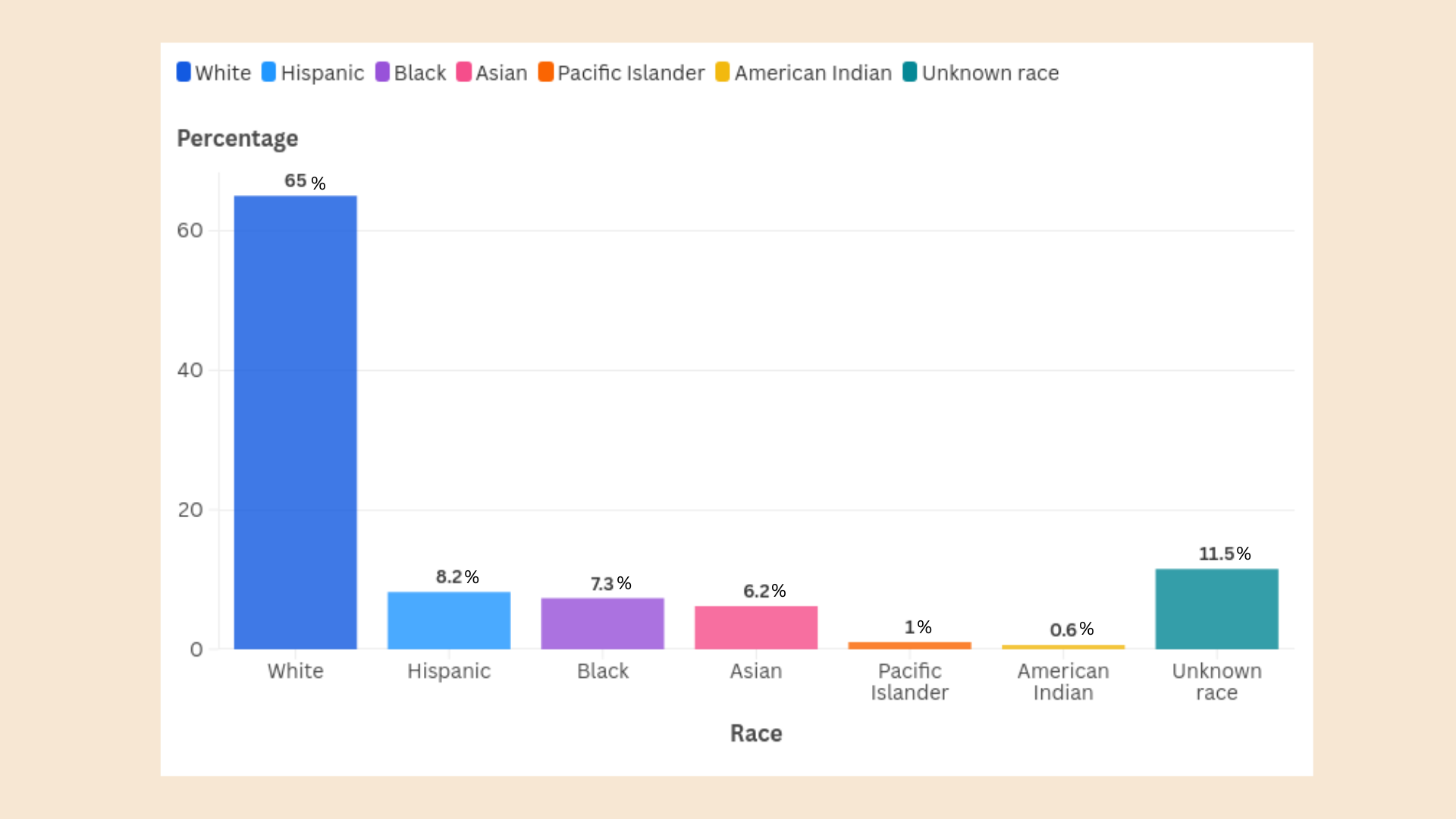
“In the US, almost 72% of patients diagnosed with endometriosis are white and only around 5% are black. This discrepancy is staggering, especially considering there’s no definitive evidence endometriosis is more common in white patients.”
Black women are commonly diagnosed for having Pelvic Inflammatory Disease (PID) which is caused by sexually transmitted infections like chlamydia and gonorrhea, vastly differing from endometriosis. A study was conducted by the American Journal of Obstetrics which reported that 40% of Black women who were diagnosed with PID actually had endometriosis.
“In the US, almost 72% of patients diagnosed with endometriosis are white and only around 5% are black. This discrepancy is staggering, especially considering there’s no definitive evidence endometriosis is more common in white patients.”
It is more common for White women to be diagnosed with endometriosis than it is for Black women to be diagnosed with the condition, despite no evidence to back this up.
The Conversation article "Endometriosis: black women continue to receive poorer care for the condition" states: “In the US, almost 72% of patients diagnosed with endometriosis are white and only around 5% are black. This discrepancy is staggering, especially considering there’s no definitive evidence endometriosis is more common in white patients.”
Endometriosis has a history of being classist and racist as to why it appeared uncommon for women of color to have the disease. The majority of the studies conducted in the past resulted in White women having higher rates of having endometriosis, but the credibility of these studies are questionable since they were performed on a predominantly White population.
“Differences in endometriosis diagnosis between Black, Asian, Hispanic, and White women are likely to be synergistic with larger systemic problems related to the difficulty of receiving an endometriosis diagnosis."
From a study conducted in 2022 that shows the percentage of women based on demographic who were treated for endometriosis with laparoscopy surgery. Data visualization made by Claire Plath.
From a study conducted in 2022 that shows the percentage of women based on demographic who were treated for endometriosis with laparoscopy surgery. Data visualization made by Claire Plath.
"Oral contraceptives are not the cure" graphic made by Claire Plath.
"Oral contraceptives are not the cure" graphic made by Claire Plath.
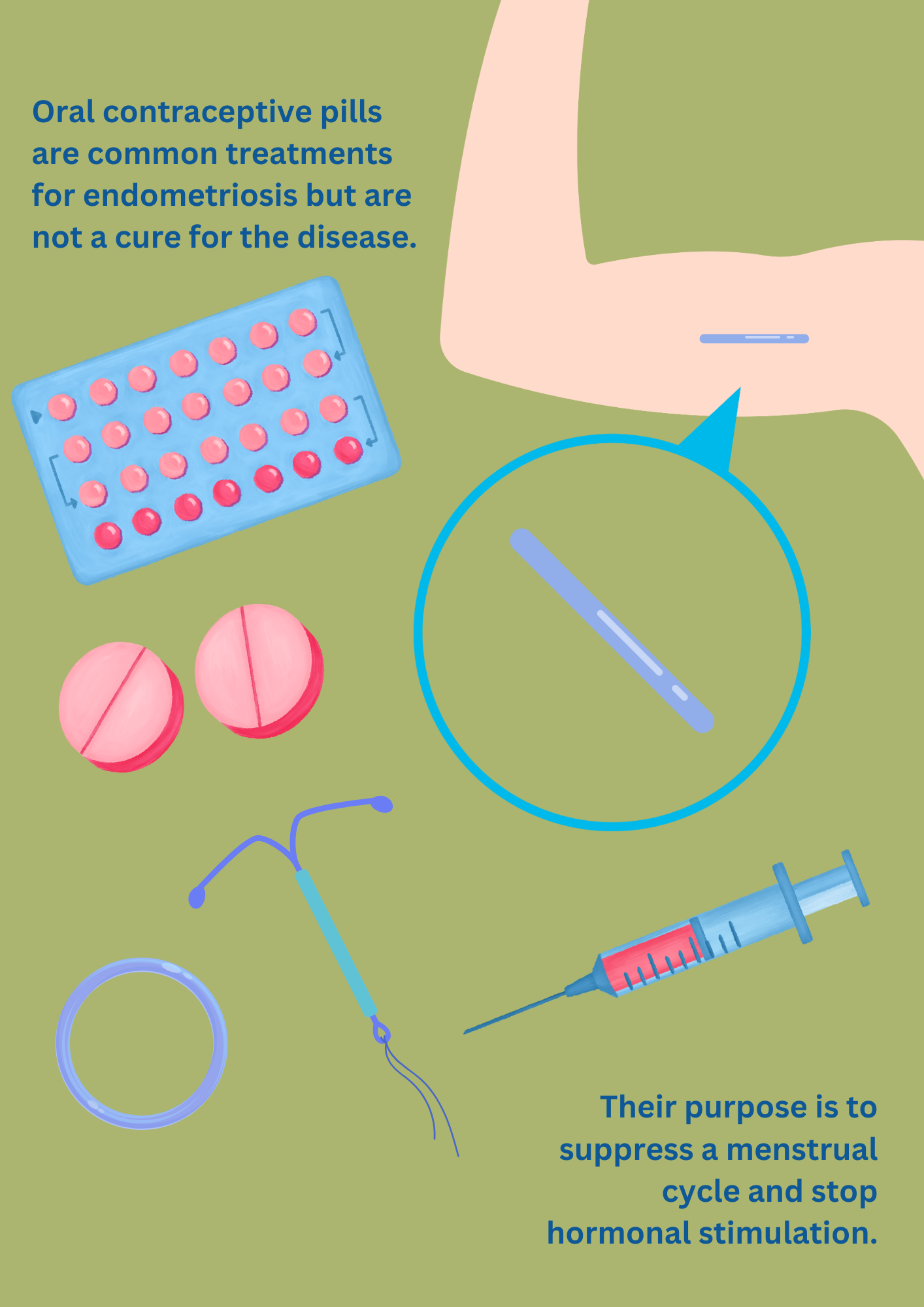
Oral contraceptive info graphic made by Claire Plath.
Oral contraceptive info graphic made by Claire Plath.
Lack of treatments
Women’s reproductive health issues are under researched. Endometriosis itself is a tough disease to diagnose and distinguish.
“The symptoms can be very broad. When you think of simple ailments that affect someone like appendicitis or pneumonia, they have very clear cut symptoms … and endometriosis is all over the board where people have recurrent, constant symptoms and severe cases with a lot of GI based symptoms,” said Dr. Kawano.
Endometriosis is not something you can diagnose reliably on imaging. There are several stages doctors go through when diagnosing endometriosis. One option includes a trans vaginal ultrasound and MRI scan on the patient, but endometriosis is often not found or detected on these scans.
"When you think of simple ailments that affect someone like appendicitis, pneumonia, they have very clear cut symptoms … and endometriosis is all over the board where people have recurrent, constant symptoms and severe cases with a lot of GI based symptoms."
“If a patient is facing an immense amount of pain, the next step will be hormonal management and menstrual suppression, usually using oral contraceptive pills, things that suppress a menstrual cycle,” said Dr. Kawano.
Oral contraceptive pills are the typical treatment for endometriosis before a laparoscopy surgery. The contraceptive pills are suppressants that help stop the hormonal stimulation from the ovaries since endometriosis is stimulated by estrogen. The simplest way to think about it is they put a woman into a temporary menopause, so it stops the hormonal stimulation to the endometriosis lesions.
It quiets it down. It slows it down. It does not stop it.
Common contraceptive (birth control) methods for treating endometriosis include:
- Pills
- Hormonal intrauterine devices (IUDs)
- Vaginal rings
- Implants
- Patches
- Injections
The downside? These treatments should not be used long term for endometriosis as they can have long-lasting impacts on a woman’s well being when they are taken specifically for the disease.
Every person reacts differently to treatments. Some methods may work for a woman while some may not. Progesterone-only contraceptives are options for women with endometriosis and can help alleviate symptoms. However, they can also have their own side effects that can make it worse for women who are enduring endometriosis.
Symptoms women with endometriosis may experience when taking progesterone-only contraceptives include:
- Irregular bleeding patterns
- Functional ovarian cysts
- Mood changes
- Acne
- Weight gain
- Cramping
- Breast tenderness
To name just a few.
The most definite way to find endometriosis is through a laparoscopy surgery which involves filling the belly with gas which creates open space, instead of just seeing the organs squished together when surgically opened up. With this magnification, doctors are able to look at all of the surfaces of the organs, where they are able to notice the endometriosis (which resembles blisters) spreading on the organs. Surgical advancements have allowed doctors to identify and understand the disease at a clearer level.
The issue rests on the fact that surgery is typically the last option. You can go in and do surgery but you may end up in the same exact place afterwards.
“Surgery is risky in the grand scheme of things. You want to use surgery as the last resort. The other thing is, surgery is not always curative of endometriosis. It can treat it and temporize symptoms but does not cure it, and so you have to be very careful,” explained Dr. Kawano.
Women who have passed their childbearing years or do not plan to have children, can decide to go through a hysterectomy as a treatment method for endometriosis. A hysterectomy is not a cure for endometriosis, but it does suppress the pain.
“A lot of women undergo a hysterectomy for management of their symptoms. I think it helps a lot of women, since endometriosis is not really something you deal with after menopause because it is mostly all hormonally stimulated,” said Dr. Kawano.
"People who are going to doctors who don't fully understand how endometriosis can present itself, their symptoms are then downplayed or minimized or overlooked, and it leaves women feeling like they are crazy and that nobody is listening to them.”
Lack of research
Endometriosis is an under researched and undermined disease. There is far less research funding for women’s reproductive health compared to other forms of research.
The article “Understanding Endometriosis Underfunding and its Detrimental Impact on Awareness and Research” published in npj Women’s Health in 2024, dives into the disparities that women with endometriosis face because it is substantially underfunded.
In 2022, U.S. funding for endometriosis was $16 million, equating to approximately $2.00 per patient annually. In contrast, Crohn’s disease, which impacts 690,000 people in the U.S. received $90 million in research funding which translates to approximately $130 per patient.
Issues affecting women are drastically underfunded compared to male medical issues which are overfunded. Studies indicate that women are 25% less likely than men to receive pain relief, highlighting a huge flaw in the medical system and a gender bias.
If men had endometriosis like women do, would this be an issue?
Because of the lack of research, it is hard to tell what causes endometriosis and without knowing its cause, it remains incurable.
“It was a lot of being dismissed by doctors and medical professionals, which is very isolating and frustrating to experience, and unfortunately, the reality of endometriosis and women’s health in general is that women are often dismissed and their stories are just not validated or understood,” Ratelle said. And that is what I went through personally.”
When conducting interviews with medical facilities and specialties on endometriosis, it was extremely difficult to find someone to talk to who specializes in endometriosis.
When reaching out to Sharp HealthCare in San Diego to conduct an interview, this was their response: "We apologize that we were not able to locate anyone that is available to do this interview," showing evidence on the lack of awareness on women's reproductive health.
Graphic made by Claire Plath.
Graphic made by Claire Plath.
Treatment advancements
Despite the negative effects and history that come with endometriosis, there are positive steps in the right direction happening. There are a lot of advancements with robotics surgery and technology to better identify endometriosis that allow medical professionals to treat endometriosis more accurately and remove the tissue.
More holistic methods are arising to relieve endometriosis pain including physical activities like yoga, heat therapy, herbal supplements and acupuncture.
There is an improvement in attention to it than there was 10 years ago that needs to continue to rise. More women are feeling comfortable and confident to have these difficult discussions and bring awareness to the matter. Social media has become a platform for women to advocate for endometriosis openly.
The article “Holistic Approaches in Endometriosis - as an Effective Method of Supporting Traditional Treatment: A Systematic Research and Narrative Review” published in 2024 by Reproductive Sciences explores holistic approaches to alleviate endometriosis symptoms women with the disease can try.
“It was emphasized that yoga techniques, particularly breathing exercises, were beneficial in coping with pain, leading to reduced reliance on painkillers. Yoga also fostered self-control, self-awareness, autonomy, improved sleep, better management of panic attacks, and increased self-confidence.”
Integrating holistic methods into endometriosis treatment can improve a woman’s symptoms and is a different approach compared to contraceptive methods. Treatment plans depend on the person, what their body responds to and what is a best fit for them.
Ratelle recounted that one of the most beneficial ways to manage her pain has been acupuncture and physical activity like yoga and adult ballet classes. She also emphasized the importance of advocating for yourself.
“Listen to your gut, trust yourself, trust your instincts and advocate for the care that you deserve,” said Ratelle. “Do your research and don’t shy away from, you know, people telling you what you are feeling is not real because it is real and you are not alone.”
To the women who are feeling let down and not heard, to the women who are feeling pain and are being dismissed, the most important thing is to stand up for yourself.
“I think it is continuing to advocate for yourself and look for a specialist,” said Dr. Kawano. “If you are not getting the answers or the help you think you need, then get another opinion and try to find a specialist. But also try to understand that not all gynecologists are going to have the thumb on this in the ways we hope they could or feel they should.”
With my endometriosis journey, I still have my ups and downs. In May 2023, I was able to undergo a laparoscopy surgery for my endometriosis, where it was discovered that my endometriosis had spread all around my lower back. I felt immensely better than I had before after getting my surgery, but there are other dark days when my pain is unbearable. I do not know what the future holds for me or whether or not my endometriosis has affected my fertility long term, but I am choosing to take it one day at a time.
From left: Cammie Plath, Claire Plath (myself) and Shirley Hackett. Photo courtesy of Cammie Plath.
From left: Cammie Plath, Claire Plath (myself) and Shirley Hackett. Photo courtesy of Cammie Plath.
It is a comfort knowing I finally got my voice loud enough to be heard.
You are not hysterical.
You deserve to be heard.